HEALTH watchdogs have told Bath and North East Somerset Council it ‘requires improvement’ in ensuring people have access to adult social care and support.
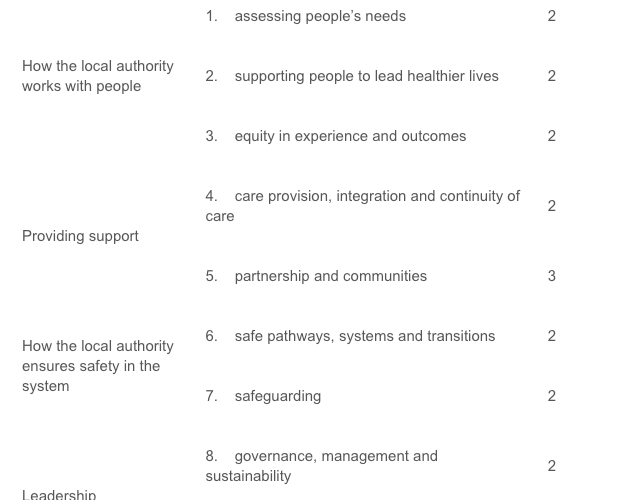
The Care Quality Commission (CQC) looked at nine different areas spread across for areas before delivering its verdict.
James Bullion, CQC’s chief inspector of adult social care and integrated care, said: “We found that people’s experiences of accessing B&NES’ adult social care services were mixed.
“We found some people were having to wait a long time to either access services or have reviews. We also saw that leaders had identified where improvements were needed to make sure plans were more person-centred and flexible to meet people’s needs.
“Over 70 per cent of people receiving long term support had been reviewed. However, some people’s care needs hadn’t been reviewed in over two years due to an increase in demand and workload.
“People told us that they could access services easily, but people who were less comfortable using digital platforms found it difficult to find relevant information online.
“The training offer was accessible, informative and relevant which helped improve the services people had access to. However, wider transformation in the organisation had caused uncertainty.

“The local authority sought people’s views and feedback to help improve services and accessibility. People using services told us that they felt listened to and respected. They said they were looking forward to seeing how their views would improve services.
“The local authority’s staff were described as kind, dedicated and passionate.
“The authority are aware of areas where improvements need to be made to provide a better experience for people using the service. We look forward to seeing the changes.”
The assessment team found:
- People said that reviews of care and carers assessments were inconsistent and on occasion relied on people contacting the local authority themselves to request a review.
- Staff said that people who didn’t require a Care Act assessment would be signposted to appropriate services, but this information wasn’t recorded. This made it harder for leaders to have an overview of this work.
- Some leaders didn’t fully understand the at-risk groups and diverse communities in their area.
- Some staff felt they had not received the correct training and guidance to work with people with more complex or specialist needs. Leaders told us that they had started to make improvements to their learning offer.
The assessment team also found:
- National data on short and long term support showed that 71.72% of people receiving long term support had been reviewed, compared to the England average of 58.77.
- People who were funding their own care were supported to find services, with approximately 60% of people needing services self-funding.
- People’s experience of adult social care services was above average according to national data.
- Staff said the training offer has improved since moving back in house and that training was easily accessible, informative and relevant to their job roles.
The full assessment has been published on the CQC’s website.

.jpeg?width=209&height=140&crop=209:145,smart&quality=75)


